- The natural host of the monkeypox virus
- Who is more prone to get affected by the monkeypox virus?
- Transmission
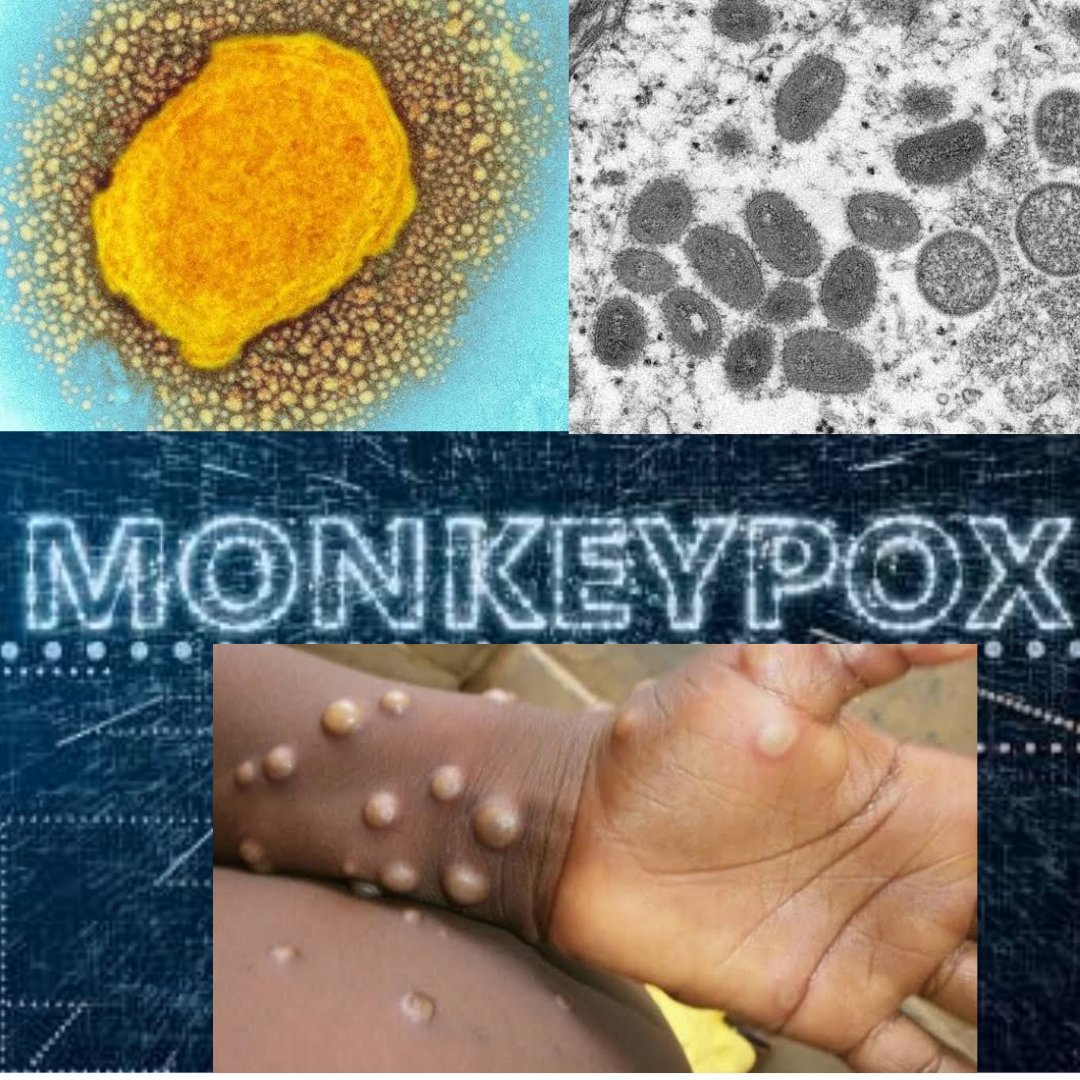
- The pathogen
- Monkeypox Disease
- symptoms
- What is the differential diagnosis of the monkeypox virus?
- homeopathic medicines for
- Monkeypox Disease
- severity of
- Monkeypox Disease
- Prevention of
- Monkeypox Disease
- Reference
Monkeypox virus was first discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research, hence the name ‘monkeypox.’ The first human case of monkeypox was recorded in 1970 in the Democratic Republic of Congo during a period of intensified effort to eliminate smallpox. Since then monkeypox has been reported in humans in other central and western African countries.
Monkeypox is a rare disease that is caused by infection with the monkeypox virus. Monkeypox virus belongs to the Orthopoxvirus genus in the family Poxviridae. The Orthopoxvirus genus also includes variola virus (which causes smallpox), vaccinia virus (used in the smallpox vaccine), and cowpox virus. (1)
The natural host of the monkeypox virus
Various animal species have been identified as susceptible to the monkeypox virus. This includes rope squirrels, tree squirrels, Gambian pouched rats, dormice, non-human primates, and other species. Uncertainty remains on the natural history of the monkeypox virus and further studies are needed to identify the exact reservoir(s) and how virus circulation is maintained in nature. (2)
Who is more prone to get affected by the monkeypox virus?
• Person coming more in contact with animals in forest area
• Immuno-comprised people
• People of all ages and both the sexes
• Generally, people younger than 40-50yrs (3)
Transmission
Transmission of monkeypox virus occurs when a person comes into contact with the virus from an animal, human, or materials contaminated with the virus. The virus enters the body through broken skin (even if not visible), respiratory tract, or mucous membranes (eyes, nose, or mouth). animal-to-human transmission may occur by bite or scratch, bush meat preparation, direct contact with body fluids or lesion material, or indirect contact with lesion material, such as through contaminated bedding. Human-to-human transmission is thought to occur primarily through large respiratory droplets. Respiratory droplets generally cannot travel more than a few feet, so prolonged face-to-face contact is required. Other human-to-human methods of transmission include direct contact with body fluids or lesion material, and indirect contact with lesion material, such as through contaminated clothing or linens.
The reservoir host (main disease carrier) of monkeypox is still unknown although African rodents are suspected to play a part in transmission. The virus that causes monkeypox has only been recovered (isolated) twice from an animal in nature. In the first instance (1985), the virus was recovered from an apparently ill African rodent (rope squirrel) in the Equateur region of the Democratic Republic of Congo. In the second (2012), the virus was recovered from a dead infant mangabey found in the Tai National Park, Cote d’Ivoire. (1)
The pathogen
Monkeypox virus is an enveloped double-stranded DNA virus that belongs to the Orthopoxvirus genus of the Poxviridae family. There are two distinct genetic clades of the monkeypox virus – the Central African (Congo Basin) clade and the West African clade. The Congo Basin clade has historically caused more severe disease and was thought to be more transmissible. The geographical division between the two clades has so far been in Cameroon – the only country where both virus clades have been found. (2)
Monkeypox virus Disease
Incubation period
Infection with the monkeypox virus begins with an incubation period. A person is not contagious during this period.
• Incubation period averages 7−14 days but can range from 5−21 days.
• A person does not have symptoms and may feel fine. (1)
symptoms
In humans, the symptoms of monkeypox are similar to but milder than the symptoms of smallpox. Monkeypox begins with fever, headache, muscle aches, and exhaustion. The main difference between the symptoms of smallpox and monkeypox is that monkeypox causes lymph nodes to swell (lymphadenopathy) while smallpox does not. The incubation period (time from infection to symptoms) for monkeypox is usually 7−14 days but can range from 5−21 days.
The illness begins with:
• Fever
• Headache
• Muscle aches
• Backache
• Swollen lymph nodes
• Chills
• Exhaustion
Within 1 to 3 days (sometimes longer) after the appearance of fever, the patient develops a rash, often beginning on the face then spreading to other parts of the body.
Lesions progress through the following stages before falling off:
• Macules
• Papules
• Vesicles
• Pustules
• Scabs
The illness typically lasts for 2−4 weeks. In Africa, monkeypox has been shown to cause death in as many as 1 in 10 persons who contract the disease. (1)
Prodrome
Persons with monkeypox will develop an early set of symptoms (prodrome). A person may sometimes be contagious during this period.
• The first symptoms include fever, malaise, headache, sometimes sore throat, cough, and lymphadenopathy (swollen lymph nodes).
• Lymphadenopathy is a distinguishing feature of monkeypox from smallpox.
• This typically occurs with fever onset, 1–2 days before rash onset, or rarely with rash onset.
• Lymph nodes may swell in the neck (submandibular & cervical), armpits (axillary), or groin (inguinal) and occur on both sides of the body or just one. (1)
Rash
Following the prodrome, lesions will develop in the mouth and on the body. Lesions progress through several stages before falling off. A person is contagious from the onset of the enanthem through the scab stage.
1. Enanthem: The first lesions to develop are on the tongue and in the mouth.
• 2. Macules: (1−2 days) Following the enanthem, a macular rash appears on the skin, starting on the face and spreading to the arms and legs and then to the hands and feet, including the palmdistributionThe rash typically spreads to all parts of the body within 24 hours becoming most concentrated on the face, arms, and legs (centrifugal distribution
• Papules: (1−2 days)By the third day of rash, lesions have progressed from macular (flat) to papular (raised).
• Vesicles: (1−2 days) By the fourth to fifth day, lesions have become vesicular (raised and filled with clear fluid).
• Pustules: (5−7 days) By the sixth to the seventh day, lesions have become pustular (filled with opaque fluid) – sharply raised, usually round, and firm to the touch (deep-seated).
• Lesions will develop depression in the center (umbilication).
• The pustules will remain for approximately 5 to 7 days before beginning to crust.
• Scabs: (7−14 days)By the end of the second week, pustules have crusted and scabbed over.
• Scabs will remain for about a week before beginning to fall off. (1)
What is the differential diagnosis of the monkeypox virus?
SMALLPOX
It is very much like smallpox, as rash and pustule presentation are very much alike, in the monkeypox virus lymph nodes are enlarged which can be a differentiating point between them. (3)
Homeopathic medicines for
Monkeypox virus Disease
Homeopathy can help in improving immunity and help to fight viral infections, it helps in relieving the pain and suffering and aids natural recovery.
Skin; eruptions; smallpox, variola: ACON(3) agar alum AM-C(3) am-m(2) ANAC(3) ANAC-OC(3) anath ANT-C(3) ANT-T(4) anthr APIS(4) ARG-N(3) ARN(3) ARS(4) BAPT(3) BELL(3) BRY(3) bufo camph(2) cann-s canth CARB-AC(3) CARB-V(3) caust cham CHIN(4) CHIN-S(3) CHLOR(3) cimic clem(2) cocc(2) coff CROT-H(3) croto-t cund CUPR(3) cupr-acet cycl eryth(2) euon gels HAM(4) HEP(3) hippoz HYDR(3) hyos(2) IOD(3) ip KALI-BI(3) kali-br kali-i kali-m KREOS(3) lac-c LACH(3) LED(3) lepro(2) lyc m-art MALAND(4) med MERC(4) merc-c merc-i-f(2) MERC-I-R(3) mill MUR-AC(3) nat-c NAT-M(3) nat-n nat-s nit-ac op petr PH-AC(3) PHOS(3) PLAT(3) psor PULS(3) pyrog RHUS-T(4) salol sanic SARR(4) SEC(3) SEP(3) SIL(3) SIN-N(3) SOL-N(3) sol-x spig STRAM(3) sul-ac SULPH(4) syph thea THUJ(4) tub VAC(4) VARIO(4) verat VERAT-V(3) verin ZINC(3). (5)
Thuja occidentalis
- Painful sensitiveness of skin.
- Itching shootings in the skin, esp. in the evening and at night.
- Purulent pimples, like variola. Pustules. Small-pox.
- Eruptions only on covered parts.
- The eruptions burn violently after scratching.
- Sycotic excrescences, smelling like old cheese, or like the brine of fish.
- Flat ulcers, with a bluish-white bottom.
- The majority of cutaneous symptoms are > by touch.
- The flesh feels as if beaten off the bones.
- A sensation of lightness of the body when walking.─
- Stitches in various parts, changing to burning.
- Tearing and pulsative pains, as if the parts affected were ulcerated.
- Inflammatory swellings, with redness.
- Affections of the r. abdominal ring; wings of the nose; loins; inguinal glands; fingers, tips of fingers; toes.
- Glandular cervical enlargements.
- Stiffness and general heaviness over the whole body, esp. in the shoulders and thighs.
- Physical weakness, with sustained mental powers.
- Aneurism by anastomosis; swelling of the blood vessels.
- Eruption of pimples on buttocks, thighs, and knees.
- Ulcers on thighs.
- Suppurating pustules on knees.
- The inflammatory red swelling in ends of toes or instep, with pain and tension when treading, and during movement.
- Nets of veins, as if marbled, on soles of feet.
- Red, marbled spots on the instep. Red marbled spots on the forearm.
- A sensation of dryness in the skin of hands.
- Red and painful swelling in fingertips.
- Small red pimples on the neck close together.
- Swelling of glands of the neck.
- Flat, white ulcers on the inside of the lips, and on the corners of the mouth.
- Aphthć in the mouth (ulcers; mouth feels as if burnt).
- Considerable swelling of salivary glands, with increased saliva in the mouth.
- Swelling of the tongue (esp. on r. side; bites tongue frequently), painful when touched. (4)
Pulsatilla nigricans
- The great sensibility of eyes to light causes lancinating pains. Inflammatory swelling, heat, and erysipelatous redness of the ear and auditory duct, as well as of surrounding external parts.
- Painful swelling of bones behind ears.Discharge from one or both ears, which may come on after measles or any other disease, or may occur spontaneously.
- Otorrhśa with throbbing tinnitus.
- The nose feels sore internally and externally.
- Ulceration of nostrils.Obstruction of the nose and dry coryza, principally in the evening and in the heat of a room.Coryza with loss of taste and smell, or with a discharge of thick yellowish-green and fetid mucus.
- Tickling in the nose and frequent sneezing, principally in morning and evening. Constant shivering during coryza.Imaginary smells. Constant smell before nose, as from coryza of long-standing, or as of a mixture of coffee and tobacco.
- Face pale or yellowish, with sunken eyes and sometimes with an expression of suffering. Painful sensitiveness of skin on the face.
- Swelling of submaxillary and cervical glands.
- Painful blister on r. side of the tip of the tongue. Edges of tongue feel sore as if scalded. Tongue greatly swollen, dorsum bright red and covered with a network of dilated and congested veins; varicose swelling on l. side of tongue. Cracks and painful vesicles on the tongue.
- Pain as from excoriation in the throat, as if it were all raw, with scraping, burning sensation, and smarting. Redness of throat, tonsils, and uvula, with sensation, as if those parts were swollen, < swallowing. Difficult deglutition, as from paralysis, or from contraction of throat. Inflammation of throat, with varicose swelling of veins.
- Swelling of glands of the neck.
- Strong desire for open air, which makes patients feel better in every way.
- Sharp drawing and jerking pains in muscles, < at night, or in bed in the evening, as well as by the heat of a room, > in the open air, and often accompanied by numbness, paralytic weakness, or hard swelling of parts affected.
- Shifting pains which pass rapidly from one part to the other, often with swelling and redness in joints.
- The shiverings increase as the pains become <. Pain as from a bruise or subcutaneous ulceration on touching parts affected. Semilateral pains and affections.
- Symptoms are generally most violent in the evening or at night before midnight, sometimes also in the morning and after a meal.
- Agitation and uneasiness throughout the body, with an inability to sleep or to enjoy repose, and constant inclination to stretch limbs.
- Sluggishness and heaviness of limbs, with paralytic weakness, a painful sensibility of joints, and tottering gait.
- Great desire to remain to lie down or sit.
- Pale skin. Itching, mostly burning or pricking (as if caused by ants’ stings), principally in evening, and at night in the heat of bed, < by scratching.
- Red spots, like morbilli, or nettle-rash.Frequent redness, even when the parts are cold.
- Eruptions from eating pork, itching violently in bed.
- Eruptions like measles.
- Suppurating wounds, pus thick and too profuse.
- Pus copious and yellow.
- Eruptions similar to varicella coniformis, with violent itching in bed.
- Blue-black swellings.
- Deep or fistulous ulcers; where there is much swelling around.Inflamed or putrid ulcers. (4)
Kalium Muriaticum
- Crusta lactea.
- Blister on the cornea.
- Felling of sand in the eyes.
- Deafness or earache from congestion or swelling of the middle ear or Eustachian tubes, with swelling of the glands, or cracking noises on blowing nose, or swallowing.
- Deafness due to throat troubles, white tongue.
- Deafness from swelling of the external ear.Granular conditions of external meatus and membrana tympani.Closed Eustachian tubes. It seems to act more on the Eustachian tube.
- Cheeks are swollen and painful.
- Faceache from swelling of face or gums. Aphthæ, thrush, white ulcers in mouths of little children or nursing mothers.
- Swelling glands about jaw and neck. Tonsils excessively swollen; stringy, tough mucus; swallowing excessively painful, even water or the softest bread; must twist his neck to get it down. Mumps, swelling of the parotid glands.
- Hawks up offensive, cheesy, small lumps.Greyish patches or spots in the throat.
- Schüssler’s principal remedy in gonorrhœa, and orchitis resulting from a suppression of the same.In bubo for the soft swelling, and in soft chancres Schüssler’s chief remedy.Gleet combined with eczema, visible or latent.
- Chief remedy in glandular swellings, and follicular infiltrations.
- Scrofulous enlargement of glands.Scurvy, hard infiltrations.
- Acne; erythema; eczema and other eruptions on the skin, with vesicles containing thick, white contents.
- Albuminoid eczema, or other skin diseases, arising after vaccination with bad vaccine lymph.
- Dry flour-like scales on the skin.Obstinate eczema, crusta lactea, scurfy eruption on head and face of little children. chilblains, eruptions connected with stomach or menstrual derangement.
- Ingrowing toenails. Congestions and inflammations, second stage, of any organ or part of the body.
- Catarrhal fever, great chilliness, the least cold air chills him through, has to sit close to fire to keep warm, and is chilly.
- Rheumatic fever; exudation and swelling around the joints. (4)
Variolinum
- Delirium with the initial fever. Vertigo.Syncope in attempting to rise.
- Forehead very hot, face red and bloated, carotids pulsating violently. Headache: with or after a chill; all overhead; particularly in forehead; severe in vertex; as if a band tightly encircled head; severe lancinating, throbbing; < with every pulsation.Intolerable pain in occiput.
- Keratitis, with small-pox and after vaccination.
- Pupils contracted. The skin of the face and neck deep dark-purple hue.Jaw falling when asleep, with trembling when aroused.
- Teeth covered with thick brown slime. Thick, dirty yellow coating on tongue. When asleep tongue protruded, black coating, when raised it is with difficulty drawn back; looks like a mass of putrid flesh.
- Throat very sore, redness of fauces.Pharynx and fauces deep purplish crimson, with gangrenous appearance; breath horribly offensive.Painful deglutition.Sensation as if throat were closed.Sensation as of a lump in r. side of throat. Food, esp. water, tastes sickish sweet.
- Soreness in pit of stomach and across epigastric region.Severe pain in præcordial region, frequent nausea and vomiting of bilious and bloody matter. As soon as he drinks milk he vomits it up.
- Thin, bloody stools.Several brown, green, at last grass-green stools, painless, loose, of intolerable fetid odour; no thirst; last stool slimy, with small quantity of blood.
- Urine: high-coloured, like brandy; turbid and offensive; stains a rose tea-colour, difficult to remove.
- Enlargement of testicle.Hard swelling of l. testicle in consequence of a contusion.
- Oppressed respiration.Asthma.Troublesome cough, with serous and sometimes bloody sputa. Hawking up thick, viscid slime, smelling bad.
- Stiffness of neck, with tense drawing in muscles, < on motion.Pain in base of brain and neck.Chills like streams of ice-water running down from between scapulæ to sacral region.Intolerable aching in lumbar and sacral region.Pain in muscles of the back like rheumatism; < on the motion.
- Hands icy cold during invasion.Swelling of arm which had been half-paralysed.
- Exanthema of sharp, pointed pimples, usually small, seldom large and suppurating, dry, resting on small red areolæ, frequently interspersed with spots of red colour, sometimes severe itching.
- Petechial eruptions.Var. 30 warded off an attack of small-pox after intense sickness of stomach had been caused by the smell of a case.Var. 1m in water every two hours, given on third day of eruption of a confluent case cut short the attack.
- Very severe chill, followed by hot fever.Intense fever, commencing with chills running down back like streams of cold water, causing shivering and chattering of teeth.Fever with intense radiating heat, burning hot to touch.Hot fever, no thirst.Very profuse, bad-smelling sweat.(4)
Malandrinum
- Frontal and occipital headache.Impetigo covering head from crown to neck and extending behind ears.Thick, greenish crusts with pale, reddish scabs, itching < in evening.
- Red stripes under eyes. Profuse, purulent, greenish-yellow discharge, mixed with blood.
- Tongue: coated yellow, with red streak down middle (typhoid); cracked and ulcerating down middle; swollen.
- Vomiting of bilious matter; nausea. Pains around umbilicus. Dark, cadaverous-smelling stool.Yellowish, foul-smelling diarrhśa.(Child constantly handles his penis.)
- Vagina closed with impetiginous crusts, yellowish-greenish-brown in colour.
- Pain along back, as if beaten. Sore pains in limbs and joints.Run-arounds on nails of hands and feet.
- Impetiginous crusts on extensor sides of forearms. Pains, esp. in l. tibia, with petechić-like patches on anterior aspect of l. leg from knee to ankle.Petechić on both thighs, < l.(Knock-knee.)
- Small-pox.Measles; also as preventive.Impetigo covering back of head, extending over back to buttock, and even into vagina; covering labić.Impetigo on extensors of forearms.
- Boils.Malignant pustule.Bad effects of vaccination (dry, harsh skin).
- Small, dusky red spots on legs, not disappearing on pressure.(4)
severity of
Monkeypox Disease
The severity of the illness can depend upon the initial health of the individual, the route of exposure, and the strain of the infecting virus (West African vs. Central African virus genetic groups, or clades). West African monkeypox is associated with milder disease, fewer deaths, and limited human-to-human transmission. Human infections with the Central African monkeypox virus clade are typically more severe compared to those with the West African virus clade and have higher mortality. Person-to-person spread is well-documented for the Central African monkeypox virus. (1)
Prevention of
Monkeypox Disease
Raising awareness of risk factors and educating people about the measures they can take to reduce exposure to the virus is the main prevention strategy for monkeypox. Scientific studies are now underway to assess the feasibility and appropriateness of vaccination for the prevention and control of monkeypox. Some countries have, or are developing, policies to offer vaccine to persons who may be at risk such as laboratory personnel, rapid response teams and health workers.
Reducing the risk of human-to-human transmission
Surveillance and rapid identification of new cases are critical for outbreak containment. During human monkeypox outbreaks, close contact with infected persons is the most significant risk factor for monkeypox virus infection. Health workers and household members are at a greater risk of infection. Health workers caring for patients with suspected or confirmed monkeypox virus infection, or handling specimens from them, should implement standard infection control precautions. If possible, persons previously vaccinated against smallpox should be selected to care for the patient.
Samples taken from people and animals with suspected monkeypox virus infection should be handled by trained staff working in suitably equipped laboratories. Patient specimens must be safely prepared for transport with triple packaging in accordance with WHO guidance for transport of infectious substances.
The identification in May 2022 of clusters of monkeypox cases in several non-endemic countries with no direct travel links to an endemic area is atypical. Further investigations are underway to determine the likely source of infection and limit further onward spread. As the source of this outbreak is being investigated, it is important to look at all possible modes of transmission in order to safeguard public health. (2)
Reducing the risk of zoonotic transmission
Over time, most human infections have resulted from a primary, animal-to-human transmission. Unprotected contact with wild animals, especially those that are sick or dead, including their meat, blood and other parts must be avoided. Additionally, all foods containing animal meat or parts must be thoroughly cooked before eating. (2)
Preventing monkeypox through restrictions on animal trade
Some countries have put in place regulations restricting importation of rodents and non-human primates. Captive animals that are potentially infected with monkeypox should be isolated from other animals and placed into immediate quarantine. Any animals that might have come into contact with an infected animal should be quarantined, handled with standard precautions and observed for monkeypox symptoms for 30 days. (2)
How monkeypox relates to smallpox
The clinical presentation of monkeypox resembles that of smallpox, a related orthopoxvirus infection which has been eradicated. Smallpox was more easily transmitted and more often fatal as about 30% of patients died. The last case of naturally acquired smallpox occurred in 1977, and in 1980 smallpox was declared to have been eradicated worldwide after a global campaign of vaccination and containment. It has been 40 or more years since all countries ceased routine smallpox vaccination with vaccinia-based vaccines. As vaccination also protected against monkeypox in West and Central Africa, unvaccinated populations are now also more susceptible to monkeypox virus infection.
Whereas smallpox no longer occurs naturally, the global health sector remains vigilant in the event it could reappear through natural mechanisms, laboratory accident or deliberate release. To ensure global preparedness in the event of reemergence of smallpox, newer vaccines, diagnostics and antiviral agents are being developed. These may also now prove useful for prevention and control of monkeypox. (2)
Update: (20/ 05/ 22- present)
Reference
- CDC
- WHO
- DR. THIND’S HOMEOPATHIC CLINIC
- John Henry CLARKE, M.D. ;A DICTIONARY OF PRACTICAL MATERIA MEDICA.
- ROGER VAN ZANDOORT; COMPLETE REPERTORY